Biohybrid Systems for Better Living
Northwestern Engineering researchers are defining the future of medicine and health through electronics and innovative materials for applications within and on the human body.

A wearable sensor system that predicts fatigue at work. A tiny implant that delivers diabetes drugs on demand. A flexible patch that optimizes the sense of touch for the visually impaired.
Through the work of Northwestern Engineering researchers, bioelectronics like these are becoming the future of medicine. These biohybrid systems use innovations in materials and mechanical structures to overcome the mismatch between hard, rigid electronic semiconductor devices and the soft, flexible tissue and organs within the human body.
The results are new platforms and capabilities that can be integrated on and within human tissue, opening up unprecedented clinical healthcare possibilities, including treating and monitoring disease, supporting work-based performance, and optimizing overall health and well-being.
Biohybrid Systems
 When Northwestern Engineering developed its new strategic vision in 2024, the leadership team developed three core pillars key to ushering engineering into the next era. One pillar, Revolutionize the Methods of Engineering, aims to help guide engineering into the future with new tools and methodologies.
When Northwestern Engineering developed its new strategic vision in 2024, the leadership team developed three core pillars key to ushering engineering into the next era. One pillar, Revolutionize the Methods of Engineering, aims to help guide engineering into the future with new tools and methodologies.
One strategic priority that falls under this pillar is biohybrid systems. These include bioelectronics, biomaterials (including nanoscale materials designed to interact with the human body in new ways), and synthetic biology systems, which reengineer cells to help tackle issues in human health. To create these systems, Northwestern engineers are developing tools and defining future methods at the interface of engineering and biology.
Implantable Device to Monitor Inflammation
Led By
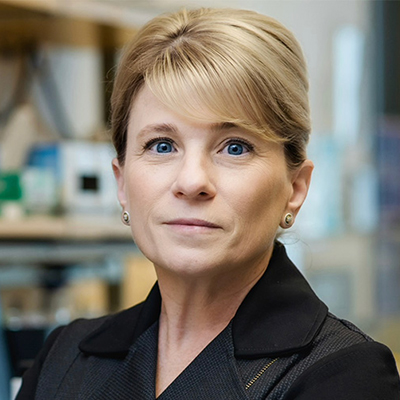
Shana O. Kelley
Neena B. Schwartz Professor of Chemistry
and Biomedical Engineering
The Problem
Although inflammation is inherent in many diseases, including cancer and heart disease, physicians currently cannot track inflammation in tissue in real time.
The Idea
A small, implantable device that can monitor fluctuating levels of proteins within the body. Inspired by fruit being shaken off tree branches, the device comprises strands of DNA that stick to proteins, shake them off, and then grab more proteins. This enables the device to sample various proteins over time and measure changes in inflammatory markers in real time.
Why It Matters
The work on this idea lays the foundation for managing and preventing acute and chronic conditions by tracking critical proteins such as cytokines in inflammation, protein biomarkers in heart failure, and many others. With continuous monitoring, physicians could fine-tune medications between visits, helping to alleviate or even prevent disease.
Haptic Patch that Stimulates Skin for Complex Sensations
Led By
 John Rogers
John Rogers
Louis Simpson and Kimberly Querrey Professor of Materials Science and Engineering, Biomedical Engineering, and Neurological Surgery
Yonggang Huang
Jan and Marcia Achenbach Professor in Mechanical Engineering and Civil and Environmental Engineering

The Problem
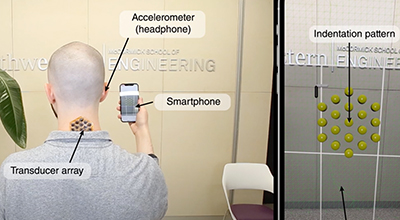
Existing haptic feedback technology, which creates the experience of touch through forces and vibrations, has limitations, especially for people with disabilities and those within virtual reality simulations.
The Idea
A thin, flexible device that adheres to skin and delivers various complex sensations and more realistic, immersive sensory experiences. The device comprises a hexagonal array of 19 small magnetic actuators encapsulated within a thin, flexible silicone-mesh material. Each actuator can deliver different sensations, including pressure, vibration, and twisting. Using Bluetooth technology on a smartphone, the device receives data about a person’s surroundings for translation into tactile feedback—substituting one sensation (like vision) for another (touch).
This sort of 'sensory substitution' provides a primitive, but functionally meaningful, sense of one's surroundings without reliance on eyesight — a capability useful for individuals with vision impairments.
John RogersLouis Simpson and Kimberly Querrey Professor of Materials Science and Engineering, Biomedical Engineering, and Neurological Surgery
Why It Matters
The device could help people with visual impairment “feel” their surroundings. The system can support a basic version of vision in the form of haptic patterns delivered to the surface of the skin based on data collected using the 3D imaging function (LiDAR) available on smartphones.
Implant to Deliver Therapy for Obesity, Type 2 Diabetes
Led By

Jonathan Rivnay
Professor of Biomedical Engineering and Materials Science and Engineering
Josh Leonard
Professor of Chemical and Biological Engineering
The Problem
More than 40 percent of US adults have obesity, and more than 35 million Americans have type 2 diabetes. Researchers are seeking novel ways to create and deliver medications to treat these widespread conditions.
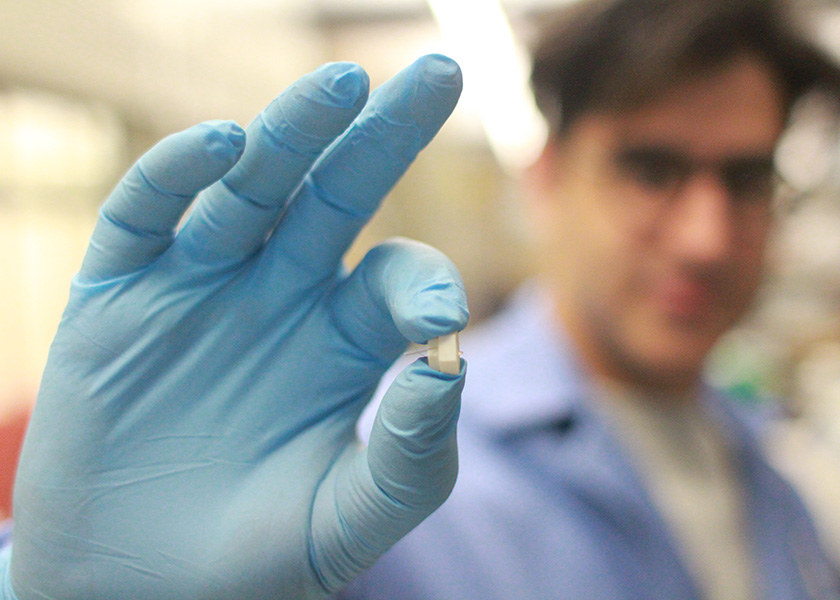
The Idea
A low-cost bioelectronic implant to treat obesity and type 2 diabetes. Rivnay and Leonard are developing “Rx On-site Generation Using Electronics” (ROGUE), an implantable device that will deliver a biological therapy on demand. Measuring only a few millimeters in diameter, the implant will house living engineered cells that synthesize and deliver therapy when needed.
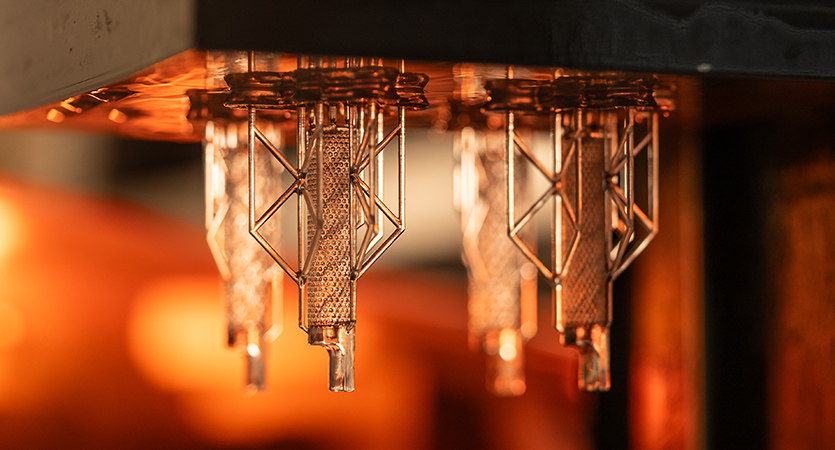
This work builds on the biohybrid work seeded at Northwestern, where we are making regulated therapies based on engineered cell factories that can be controlled and maintained by a bioelectronic device.
Jonathan RivnayProfessor of Biomedical Engineering and Materials Science and Engineering
Why It Matters
The minimally invasive living device can be implanted under the skin to deliver personalized and regulated therapies, ultimately eliminating the need for daily or weekly injections, trips to the pharmacy, and careful storage of expensive medications.
Wearable Fatigue-Prediction Sensor System
Led By
Ping Guo
Associate Professor of Mechanical Engineering
Qi Zhu
Professor of Electrical and Computer Engineering
The Problem
A 2018 National Safety Council report noted that 63 percent of manufacturing workers report feeling tired at work, which increases the risk of accidents and injuries and decreases overall performance.
The Idea
A wearable, multimodal sensor system that leverages machine learning to enable near-real-time fatigue prediction and reporting on the factory floor. The system uses soft, flexible sensors to continuously monitor locomotive skills and vital signs, including heart rate and skin temperature. The sensor data, which accounts for person-specific attributes such as age, gender, height, and weight, is transmitted to the user through a “fatigue scorecard” visual dashboard.
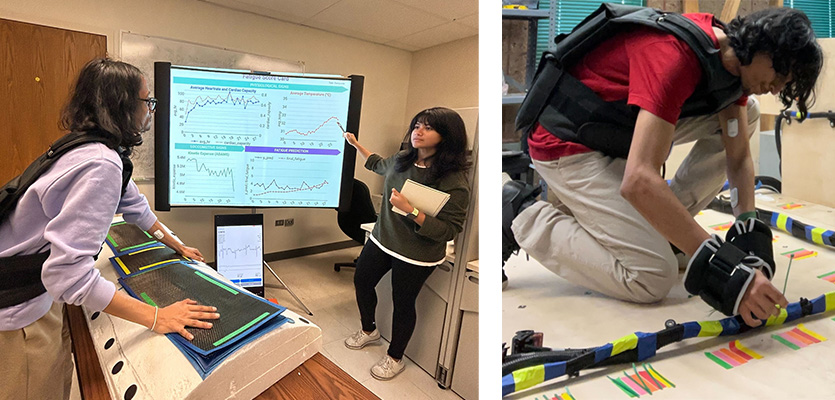
Fatigue is often oversimplified as a binary state — fatigue or non-fatigue. However, for manufacturing operators, a more nuanced approach is required. Our system relies on privacy-preserving, unobtrusive sensing modalities paired with lightweight analytics suitable for on-device deployment.
Ping GuoAssociate Professor of Mechanical Engineering
Why It Matters
The system could help manufacturers preemptively address worker fatigue and reduce operational losses. It represents a significant step toward improving worker safety with potential applications in other sectors that involve physical motion and fatigue, including sports and medicine.
Millimeter-Sized, Dissolvable Pacemaker
Led By
Igor Efimov
Professor of Biomedical Engineering and Medicine
John A. Rogers
Louis Simpson and Kimberly Querrey Professor of Materials Science and Engineering, Biomedical Engineering, and Neurological Surgery
Yonggang Huang
Jan and Marcia Achenbach Professor in Mechanical Engineering and Civil and Environmental Engineering
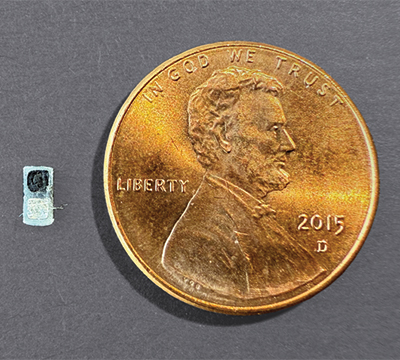
The Problem
Babies with certain congenital heart defects need temporary pacemakers after cardiac surgery, but conventional pacemakers are large and require surgery for implantation.
The Idea
A battery-powered, millimeter-sized pacemaker that can stimulate the heart autonomously. The pacemaker is smaller than a grain of rice and can be delivered through a catheter into the chest. A skin-interfaced wireless sensor, worn on the patient’s chest, allows for on-demand operation. Made of bioresorbable materials, the pacemaker dissolves in the body after use.
About 1 percent of children are born with congenital heart defects; many of them require surgery and a temporary pacemaker. Now, we can place this tiny pacemaker on a child’s heart and stimulate it with a soft, gentle, wearable device. And no additional surgery is necessary to remove it.
Igor EfimovProfessor of Biomedical Engineering and Medicine
Why It Matters
Because the device is so small and can be implanted easily, the pacemaker could work well both for young patients and adult cardiac surgery patients whose bodies are not suited to traditional pacemakers.
Electroactive Material for Wearable Technology and Implantable Medicine

Led By
Samuel I. Stupp
Board of Trustees Professor of Materials Science and Engineering, Chemistry, Medicine, and Biomedical Engineering
The Problem
Ferroelectric materials—those with polar structures that can reverse orientation using external voltage—are traditionally hard, rigid, and often made from toxic substances. This makes using them impractical in electronic systems designed to integrate with the human body, such as biomedical implants or wearable technology.
The Idea
A soft ferroelectric material made of flexible, nanosized ribbons built by thousands of molecules that could store energy or record digital information. This new material, reported in the journal Nature in October, integrates peptides with miniature molecular segments from polyvinylidene fluoride, a common plastic used in audio equipment that produces electrical signals when pressed or squeezed.
The result is a biodegradable material that requires incredibly low voltage to flip its polarity, which is useful for energy storage and in creating low-power electronics and nanoscale devices. Stupp also envisions attaching signals for cells in the peptide segments, offering a unique combination at the molecular level that generates materials that are both electrically active and bioactive.
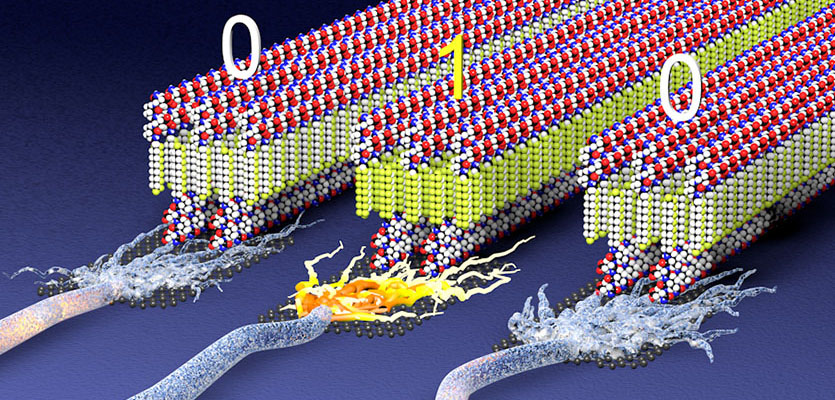
This is a wholly new concept in materials science and soft materials research. We imagine a future where you could wear a shirt with air conditioning built into it or rely on soft bioactive implants that feel like tissues and are activated wirelessly to improve heart or brain function.
Samuel I. StuppBoard of Trustees Professor of Materials Science and Engineering, Chemistry, Medicine, and Biomedical Engineering
Why It Matters
With further development, these soft materials could be used in energy-efficient microscopic memory chips, sensors, and energy storage units—technologies that could be integrated into woven fibers to create smart fabrics or to power sticker-like medical implants for treating heart or brain function.